Maritime and Coastguard Agency
Guidance
THE SHIP CAPTAIN'S MEDICAL GUIDE
First Aid
Last updated 8 July 2014Contents
- Introduction
- Priorities
- General principles of first aid on board ship
- General assessment of the situation
- Dressings, bandages, slings and splints
- First aid satchels or boxes
- Severe bleeding
- Unconscious casualty
- Burns and scalds
- Suffocation (Asphyxia)
- Strangulation
- Choking
- Epileptic fits - convulsions
- Shock and circulatory collapse
- Bleeding
- Wounds
- Fractures
- Dislocations
- Head injuries
- Chest injuries
- Blast injuries
- Transportation
Introduction
When a ship is in port, or near to port where hospital and other expert medical attention are available, the first aid treatment necessary aboard ship is similar to that practised ashore. At sea, in the absence of these facilities, trained ships' officers are required to give types of treatment beyond that accepted as normal first aid
The content of this chapter covers the knowledge of first aid necessary for the safe and efficient immediate treatment of casualties before they are transported to the ship's hospital or to a cabin for any necessary definitive treatment of the type described in chapter The care and treatment, after first-aid
However, anyone aboard ship may find a casualty and every seaman should know three basic life-saving actions to be given immediately while waiting for trained help to arrive. These are:
- to give artificial respiration by the mouth to nose/mouth method;
- to place an unconscious casualty in the unconscious position;
- to stop severe bleeding.
Priorities
On finding a casualty:
- ensure your own safety;
- give immediate treatment to the casualty who is not breathing and/or whose heart has stopped, is bleeding severely or unconscious – others can be treated later;
- send for help.
- send for help;
- treat the most serious injury first in the order of:
- not breathing and/or heart stopped;
- unconsciousness.
- serious bleeding;
- DO NOT enter the enclosed space unless you are a trained member of a rescue team acting under instructions;
- send for help and inform the master.
General principles of first aid on board ship
The general principles are:
- make a rapid examination of the patient to assess responsiveness and the extent of the injury;
- check breathing, heart and look for serious bleeding;
- if breathing has stopped, give artificial respiration;
- if the heart has stopped, give heart compression and artificial respiration;
- arrest serious bleeding; - handle the patient as little and as gently as possible so as to:
- prevent further injuries; and
- prevent further shock; - see that the patient is put in the most comfortable position possible and loosen tight clothing so that he can breathe easily;
- do not remove more clothing than is necessary and, when you do, remove it gently. With an injured limb, get the sound limb out of the clothing first and then peel the clothes off the injured limb, which should be supported by another person during the process. If cutting clothes is indicated to expose the injured part, do so. In removing a boot or shoe remove the lace and, if necessary, cut the upper down towards the toecap; keep onlookers away.
- always remember that shock can be a great danger to life and one of the main objects of first aid is to prevent this;
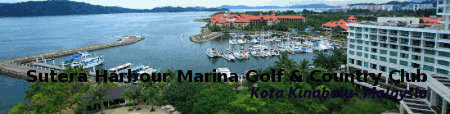
- you may have to improvise splints, bandages etc. (Figure 1.23);
- do not give alcohol in any form;
- do not move the patient until he is fit to be moved. Bleeding should be arrested, fractures immobilised and shock treated. See that the necessary personnel and equipment for smooth and efficient transport are available;
- never consider anyone to be dead until you and others agree that:
- breathing has stopped;
- no pulse is felt and no sounds are heard when the examiner's ear is put to the chest;
- the eyes are glazed and pupils are dilated;
- there is a progressive cooling of the body.
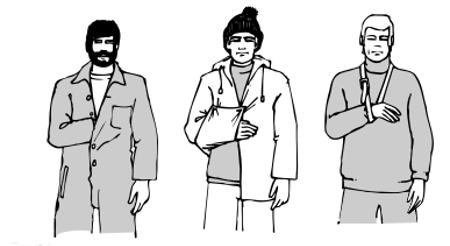
Figure 1.23
General assessment of the situation
Once it has been established that there is no immediate threat to life there will be time to take stock of the situation. Reassurance and quick and effective attention to injuries and compassionate treatment of the injured person will alleviate his condition. Remember:
- a calm and systematic approach should be adopted;
- give nothing by mouth;
- protect the casualty from heat or cold, remembering that in the tropics open steel decks can be very hot;
- never underestimate and do not treat as minor injuries:
- unconsciousness
- suspected internal bleeding
- stab or puncture wounds
- wounds near joints (see fractures);
- possible fractures
- eye injuries
Dressings, bandages, slings and splints
Standard dressing
A standard dressing consists of a thick pad of gauze which is attached to a bandage, leaving about 30cm of tail. The dressing is packed in a paper cover and is sterile. Therefore, when the
package is opened, it is important that the gauze pad should not be allowed to touch anything (including your fingers) before it is applied to the wound.
Standard dressings are available in three sizes:
- Small Gauze pad measures 7.5 cm by 10 cm.
- Medium Gauze pad measures 10 cm by 15 cm.
- Large Gauze pad measures 15 cm by 20 cm.

Figure 1.1
Bandages
Bandages are required to apply and maintain pressure on a wound to stop bleeding, to keep a dressing in place, to provide support, and to prevent movement. Wherever a standard dressing is not used it is customary to cover a wound in the following ways:
- dry dressing – sterile gauze or lint covered by a layer of cotton wool and held in place by a roller or triangular bandage;
- non-stick dressing – sterile paraffin gauze covered by sterile gauze or lint and cotton wool and held in place as above.
Tube gauze finger bandage
Cut off a piece of tube gauze bandage 60 cm long. Lay this on a flat surface and make a longitudinal cut at one end 10 cm long through both thicknesses of the bandage (Figure 1.2). The tails so formed, 'B', will be used to secure the bandage.
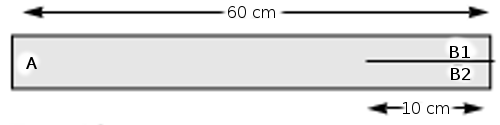
Figure 1.2
Insert the applicator into the bandage at end 'B', then push all the bandage on to it. Then pull 2.5 cm of the bandage off the end of the applicator (Figure 1.3). Tuck this inside.
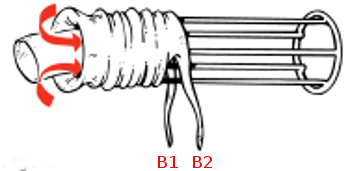
Figure 1.3
Hold the finger dressing in place. Insert the finger into the applicator and push it gently towards the base of the finger. Hold the bandage in place with your thumb and withdraw the applicator with a slight turning motion. The bandage will slip off the applicator and will mould firmly to the finger (Figure 1.4).
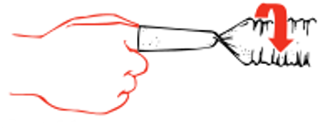
Figure 1.4
When the applicator comes off the finger, hold the bandage and the applicator firmly and turn through 360 degrees (Figure 1.5).

Figure 1.5
Re-insert the tip of the finger into the applicator and push it once again to the base of the finger (Figure 1.6).
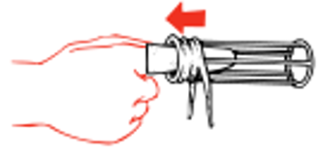
Figure 1.6
Repeat the complete manoeuvre until the bandage is all used up. Then tie loosely at the base of the finger (Figure 1.7). Tape the base of the dressing avoiding encircling the finger.

Figure 1.7
Triangular bandage
This is the most useful bandage in first aid. It can be used as a broad or narrow fold bandage to hold dressings in place. It can also be used for immobilising limbs or as a sling. It is made from calico or similar material by cutting diagonally across a square of material having 1 metre sides.The ends should always be tied with a reef knot.
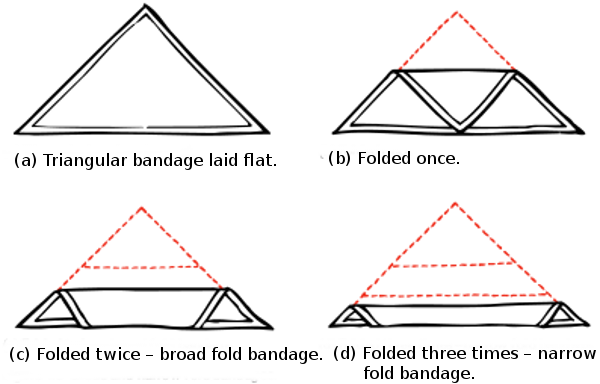
Figure 1.8
Broad and narrow fold bandages
Figure 1.8 shows how to make a broad and a narrow fold bandage. The main ways in which a triangular bandage can be used, either as a temporary dressing or to secure or cover a proper dressing, are as follows:
Hand bandage
See Figure 1.9(a) Place the hand on the bandage. Bring down point 'C' over the back of the hand to the wrist
(b) Turn 'A' over the back of the hand, under 'B' and half around the wrist.
(c) Turn 'B' over the back of the hand, over 'A' and half around the wrist.
(d) Take turns with 'A' and 'B' round the wrist and tie off.

Figure 1.9 Hand bandage
Wrist and palm bandage
Place palm on the middle of a narrow fold bandage. Take the ends and cross the bandage at the back of the hand, leaving out the thumb. Take turns of the bandage round and round the wrist and tie off at the back (Figure 1.10).

Figure 1.10
Elbow bandage
Fold over the base of the bandage and place the back of the elbow in the middle of the bandage so that the point lies at the back of the upper arm. Take the ends of the bandage round the forearm, cross them in the bend of the elbow, and then take them round the upper arm – to make a ‘figure of eight’. Tie off at the back of the arm about 10 cm above the elbow. Fold down the point and fix it with a safety pin (Figure 1.11)

Figure 1.11
Shoulder bandage
Stand facing the casualty's injured side. Place the centre of an open bandage on his shoulder with the point running up the side of the neck (Figure 1.12a). Fold a hem inwards along the base, carry the ends round the middle of the arm, cross and tie them on the outer side (Figure 1.12b). This will secure the lower border of the bandage. Apply an arm sling. Turn the point of the shoulder bandage already applied down over the knot of the arm sling. Pull it tight and pin it in place (Figure 1.12c).

Figure 1.12
Crutch bandage
Tie a narrow fold bandage round the waist; at the middle of the back pass another one under it and allow ends to hang down at the same level. Grasp both these ends and bring them forward under the crutch. Pass one end under the waist bandage in front and tie off (Figure 1.13).
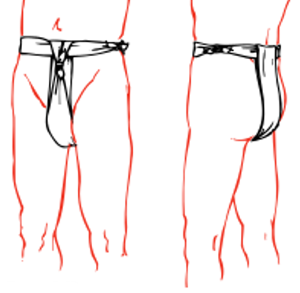
Figure 1.13
Hip bandage
Tie a narrow fold bandage round the waist with the knot on injured side. Pass the point of another bandage up under the knot, turn a fold at the base of the bandage and bring the ends round the thigh to tie off on the outer side. Pull the point up to remove creases and then fold it down over the knot and fix with safety pin (Figure 1.14).
Knee bandage
Place the point of the bandage in the front of the middle of the thigh, turn a fold at the base of the bandage so that it is about 10 cm belowthe kneecap. Take the ends round the back of the joint in a figure-of-eight and tie off in front well above the kneecap. Fold the point down over the knot and fix with safety pin (Figure 1.15).

Figure 1.14 Figure 1.15
Foot bandage
Lay the foot flat on the bandage. Bring point 'A' up over the foot in front of the ankle. Take 'B' over the foot and behind the ankle. Do the same with &apos'C'. Knot in front of the ankle (Figure 1.16).
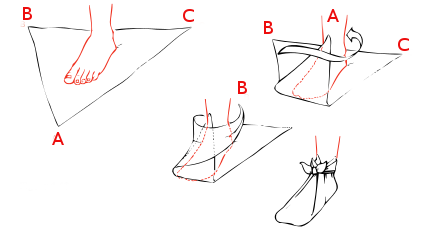
Figure 1.16
Eye bandage
Place the middle of a narrow fold bandage diagonally across the affected eye so as to cover the dressing. Take both ends round the head, cross them at the back and bring them forward again. Tie off over the forehead but not over the eye (Figure 1.17).

Figure 1.17
Head and scalp bandage
Figure 1.18 is self-explanatory. It is important that the bandage is placed just above the eyebrows. The tails 'B' and'C' should be taken well under the occiput (the bump on the back of the head where the neck joins the head), and pulled fairly tight before taking them round to the front to be tied off. Failure to do this will result in the bandage falling off, if the patient should bend over (Figure 1.18).
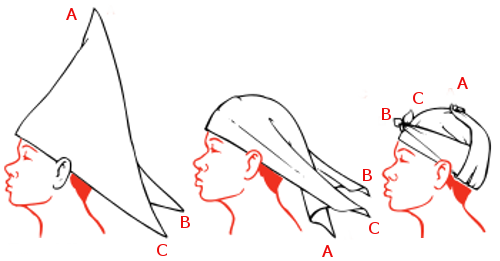
Figure 1.18
Ring pad
Spread all the fingers of one hand to form a rough circle of the required size. Make two turns of a narrow fold bandage round the ends of the fingers. Twist the remainder of the bandage round the circle so formed to make a grommet (Figure 1.19).
To pass a narrow-fold bandage under the legs or body when the casualty cannot be moved – Obtain a long piece of wood or a splint. Lay the narrow fold bandage on a flat surface. Place the splint on top of it. Then fold about 22 cm of the bandage back over the splint. Holding the splint and the bandage firmly, gently push the whole under the patient where it is required and carry on pushing until the end comes out on the opposite side. Free the bandage and draw it through. Withdraw the splint. Make the necessary tie.
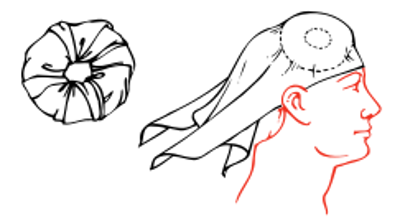
Figure 1.19
Slings
Slings are usually made from triangular bandages, or they can be improvised. The main ways in which to make a sling are as follows:
Large arm sling
Place the triangular bandage on the chest, carrying the point behind the elbow of the injured arm. One end is then placed over the shoulder of the uninjured side and the other hangs down. Gently settle the arm across the bandage, turn up its lower end over the forearm and tie it over the shoulder of the uninjured side so that it fully takes the weight of the forearm. Finally fold the point over the elbow and pin it in place (Figure 1.20).
Collar and cuff sling
This is used to support the wrist. To apply a collar and cuff sling, bend the casualty's elbow to a right angle. Pass a clove hitch round his wrist. Move his forearm across his chest with his fingers touching his opposite shoulder. Tie the ends of the bandage in the hollow just above the collarbone (Figure 1.21).

Figure 1.20 Figure 1.21
Triangular sling
This keeps the hand well raised and, with a pad under the arm, is used to treat a fracture of the collar bone (Figure 1.22). Place the casualty's forearm across his chest so that his fingers point towards the shoulder and the centre of the palm rests on the breast bone. Lay an open bandage on the forearm with one end ((C) over the hand and the point well beyond the elbow (A). Steady the limb and tuck the base of the bandage well under the hand and forearm so that the lower end ((B) may be brought under the bent elbow and then upwards across the back to the uninjured shoulder, where it is tied to end ((C) in the hollow above the collar bone. The point of the bandage ((A) is then tucked well in, between the forearm and bandage in front, and the fold thus formed is turned backwards over the lower part of the upper arm and pinned.
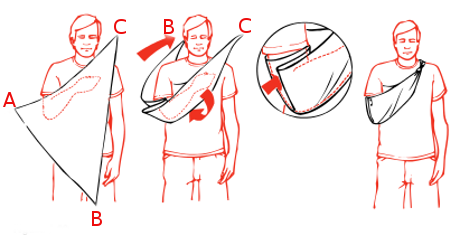
Figure 1.22
Improvised slings and supports
The affected hand or arm can be supported, when no sling is readily available, by simple methods, some of which are illustrated in Figure 1.23
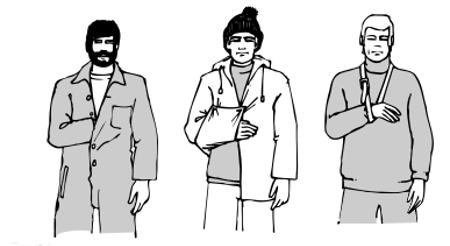
Figure 1.23
Splints
Sets of splints of various lengths are included in ships' stores. When properly applied to a limb, they relieve pain by immobilising the fracture and prevent further damage to the surrounding muscles, blood vessels and nerves. The sharp ends of the bone are prevented from piercing the skin and turning a closed fracture into an open fracture with its attendant dangers. When choosing a splint it should be long enough almost to reach the joint below and the joint above the site of the fracture. The only exception to this rule is the splint used in fractures of the thigh bone. This should be long enough to stretch from the ankle to the armpit. All splints must be fixed to the limb in at least four places – above and below the site of the fracture and at both ends. Although wooden splints are generally used in first aid, substitutes can be used in emergency situations. These can be in the form of suitably sized pieces of wood or metal, folded cardboard, newspapers or magazines, or pieces of stick or broom handles fastened together to give the necessary width. Whatever is used, the splint must be padded so that there is a layer of soft material about 1 1/2 cm thick between the splint and the skin. Unpadded splints will cause pain and possible damage to the skin.
Inflatable splints are a useful method for temporarily immobilising limb fractures but are unsuitable for fractures which are more than a short distance above the knee or elbow as they cannot provide sufficient immobilisation in these places. The splint is applied to the limb and inflated by mouth. Other methods of inflation can make the splint too tight and thus slow down or stop the circulation. Inflatable splints can be applied over wound dressings. The splints are made of clear plastic and any bleeding from a wound can easily be seen. Needless to say, all sharp objects and sharp edges must be kept well clear of the plastic to avoid a puncture.
Inflatable splints may be used to transport a patient about the ship or during moving to hospital. They should not be left in place for more than a few hours. Other means of immobilising the fracture should be used after that period. Remember that the sound leg is a very good splint to which an injured leg can be secured pending more elaborate measures, and, similarly, the arms can be immobilised against the trunk. If the patient is to be moved by Neil Robertson stretcher, no additional splints may be necessary during first aid.
First aid satchels or boxes
These should contain at least the items required by for the 'first aid kit'. One should be kept close to the ship's medical store for swift transfer to the site of an accident. If you have more than one, the other(s) should be placed away from the medical store so that if the store is destroyed by fire you have an easily reached first aid kit. These kits should be checked frequently and re-stocked as required.
Severe bleeding
- lay the casualty down;
- press where the blood comes from, using a clean handkerchief, dressing or cloth;
- press with your hand or fist on the wound if nothing else is available. If possible wear disposable gloves.
- if the arms or legs are wounded, lift them up to a near vertical position as this will help to stop the bleeding (Figure 1.24);
- tie a dressing firmly round the wound to maintain the pressure;
- if blood continues to come through the dressing, apply another bandage on the top of the first one. Bandage more firmly.
- keep the injured part as still as possible and the casualty at rest because movement disturbs (and destroys) the blood clot;
- after bleeding has been controlled, rest the limb as shown in Figure 1.24;
- this treatment applies equally to bleeding from an amputation site. Here pressure should be applied over and around the end of the stump.
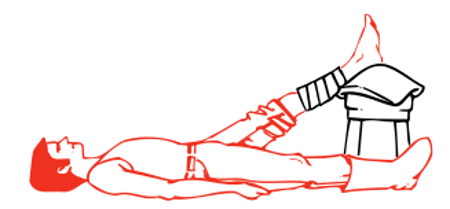
Figure 1.24
Unconscious casualty
The immediate threat to life may be:- breathing obstructed by the tongue falling back and blocking the throat;
- stopped heart
Check for breathing at once – Look/Listen/Feel
- look for movements of the chest and abdomen;
- feel for air on your cheek
- listen for breathing with your ear over the mouth and nose (Figure 1.25);
- note the colour of face and lips – normal or blue/greytinge?

Figure 1.25
If breathing:
- place the casualty in the unconscious or recovery position (Figure 1.26); NOTE: no pillows should be used under the head;
- pull up the leg and the arm on the side to which the head is facing, pull up the chin;
- stretch other arm out as pictured

The unconscious position
Figure 1.26
Not breathing:
- With the casualty lying flat on his back, open the airway by making sure that the head is tilted back whilst lifting the chin upwards and forwards (Figure 1.27), which will move the tongue forward and clear the airway.
- Open the mouth and mop out any obvious obstructions such as blood, vomit or secretions. If dentures are worn only remove them if they are broken or displaced. Use your fingers, a handkerchief or a clean piece of cloth. These actions may relieve the obstruction to breathing.
The casualty may gasp and start to breathe naturally. If so, place in the unconscious position.

Figure 1.27
Still not breathing:
Begin artificial respiration at once – seconds count.- Open the airway by making sure that the head is tilted back whilst lifting the chin upwards and forwards.
- work from the side in a convenient position;
- pinch the casualty's nose with your index finger and thumb. After taking a full breath, seal you lips about the patient's mouth and blow into his mouth until you see the chest rise. This should take about 2 seconds for full inflation. (Figure 1.28)
- give two effective inflations quickly, then note if the colour of the face and lips is improving.

Figure 1.28
If there is improvement:
- continue the artificial respiration, maintaining a rate of about a dozen inflations each minute. It may help your timing to count to five, slowly, between inflations;
- see section above on 'If breathing'.
If there is no improvement:
- listen for heart sounds (Figure 1.29);
- feel the pulse at the neck (Figure 1.29);

Figure 1.29
If no heart beat is felt, the heart has stopped. A trained first-aider must begin chest compression at once. Unless circulation is restored, the brain will be without oxygen and the person will be dead in four to six minutes:
- the casualty must be lying on his back on a hard surface, e.g. deck, otherwise the compression will be lost;
- place your hands together as shown in Figure 1.30;
- press (1/2 second duration, 100 times a minute) firmly and rapidly on the middle of the lower half of the breast bone sufficient to produce a downward movement of about 4 cm (Figure 1.31);
- artificial respiration (Figure 1.30) must also be carried out when giving heart compression since breathing stops when the heart stops. It can be given by one person, alternately compressing 15 times and then filling the lungs with air twice or, ideally, by two people – one giving heart compression and the other giving artificial respiration, at a ratio of 5 chest compressions to 1 lung inflation;
- if the heart starts to beat the colour of the face and lips will improve and the eye pupils will get smaller;
- listen again for heart sounds and feel for a neck pulse. If they are heard, stop heart compression but continue with artificial respiration until natural breathing is restored.

Hard surface
Figure 1.30

Figure 1.31
When you are satisfied that the heart is beating and unassisted breathing is restored, transfer the casualty by stretcher, in the unconscious position, to the ship’s hospital or a cabin for further treatment.
Unfortunately these measures are not always successful. Failure to restart the heart after cardiac arrest is common even in the best environment, such as a fully equipped hospital. It may be necessary to decide to stop artificial respiration and chest compression. If in doubt SEEK RADIO MEDICAL ADVICE.
Burns and scalds
Clothing on fire
- by far the best way to put out a fire on a person is to use a dry powder fire extinguisher at once;
- if a dry powder extinguisher is not available, then lay the person down and smother the flames by wrapping him in any available material (not made of man-made fibre), or throw buckets of water over him, or use a hose;
- make sure all smouldering clothing is extinguished.
NOTE: The powder from a fire extinguisher will not cause much, if any, eye damage. Most people shut their eyes tightly if sprayed with powder. Any powder which gets in the eye should be washed out immediately after the fire has been extinguished and while cooling is being undertaken.
Heat burns and scalds
- all heat burns should be cooled as quickly as possible with running cold water (sea or fresh) for at least ten minutes, or by immersing in cold water and keeping the injured part in motion; cooling of extensive burns (>15%) should be avoided as hypothermia will result.
- if it is not possible to cool the burn on the spot, the casualty should be taken to where cooling can be carried out;
- try to remove clothing gently but do not tear off any which adheres to the skin;
- then cover the burned areas with a dry, non-fluffy, dressing which is larger than the burns and bandage in place;
- further treatment as in Chapter The care and treatment, after first-aid
Electrical burns and electrocution
- make sure you do not become the next casualty when approaching any person who is in contact with electricity:
- if possible, switch off the current;
- otherwise, insulate yourself. Remove your watch and rings, wear rubber boots or stand on an insulating mat, thick DRY newspaper or wood;
- alternatively, pull the casualty from the source of supply with an insulated flex or push him away with a strong non-conductor, such as a piece of DRY wood;
- check immediately for breathing and heartbeat:
- if not breathing, give artificial respiration;
- if heart is stopped, give chest compression and artificial respiration;
- send for help;
- when the casualty is breathing, cool any burned areas and apply a clean, dry, non-fluffy covering to the burned area.
Chemical splashes
- remove contaminated clothing. Drench with water to wash the chemical away;
- carry on washing for at least ten minutes. If you are in any doubt that the chemical has been completely cleared from the skin, repeat the washing for a further ten minutes;
- give priority to washing the eyes if affected, as they are particularly vulnerable to chemical splashes. If only one eye is affected, incline the head to that side to prevent the chemical from running across into the other eye.
Suffocation (Asphyxia)
Suffocation is usually caused by gases or smoke:- remember that dangerous gases may have no smell to warn you of their presence;
- do not enter enclosed spaces without the proper precautions;
- do not forget the risks of fire and/or explosion when dealing with inflammable gases or vapours;
- get the casualty into the fresh air;
- give artificial respiration if not breathing;
- chest compression may be required if the heart stops;
- when breathing is restored, place in the unconscious position;
- oxygen may be administered later if carried on board.
Strangulation
- Immediately remove the cause;
- treat as for suffocation above;
- give protective supervision if there is any reason to suspect that the injury was self-inflicted.
Choking
Choking is usually caused by a large lump of food which sticks at the back of the throat and obstructs breathing. The person then becomes unconscious very quickly and will die in 4 to 6 minutes unless the obstruction is removed.
Choking can be mistaken for a heart attack. A person who is choking:- may have been seen to be eating;
- cannot speak or breathe;
- will turn blue and lose consciousness quickly because of lack of oxygen;
- can signal his distress (he cannot speak) by grasping his neck between fingers and thumb. This is known as the 'Heimlich sign' and, if understood by all personnel, should reduce the risks involved in choking (Figure 1.32).

Figure 1.32
Up to five firm slaps on the back, between the shoulder blades, may dislodge the obstruction. If not:
If the casualty is conscious, stand behind him, place your closed fist against the place in the upper abdomen where the ribs divide and grasp your fist with the other hand. Press suddenly and sharply into the casualty's abdomen with a hard quick upward thrust, five times if necessary. If unsuccessful continue in cycles of five back blows to five abdominal thrusts. (Figures 1.33 and 1.34).

Figures 1.33 Figures 1.34
If the casualty is unconscious, place him face upwards, keeping the chin well up and the neck bent backwards. Kneel astride him, place one hand over the other with the heel of the lower hand at the place where the ribs divide. Press suddenly and sharply into the abdomen with a hard, quick upwards thrust. Repeat several times if necessary (Figure 1.35). When the food is dislodged remove it from the mouth and place the casualty in the unconscious position.

Figures 1.35
Epileptic fits – convulsions
The fit may vary from a momentary loss of consciousness (petit mal) in which the patient may sway but does not actually fall, to a major attack (grand mal) as follows: the patient suddenly loses consciousness and falls to the ground, possibly with a cry; he remains rigid for some seconds, during which he stops breathing and the face becomes flushed; the convulsion then starts with irregular, jerky movements of the limbs, rolling of the eyes, gnashing of the teeth, with perhaps some frothing at the mouth. He may lose control and pass urine or faeces. After a variable time, but usually in a few minutes, the convulsion ceases and he falls into what appears to be a deep sleep.
Treatment
- prevent the patient from hurting himself in the convulsive stage;
- never restrain him forcibly, as this may cause injury, but remove hard objects and surround him by pillows, clothing or other soft material;
- after the fit is over, check for injuries. Assuming the patient is uninjured, let him sleep it off. He may be rather confused and dazed when he comes round. Reassure him and do not leave him until you are sure he is aware of his surroundings and knows what he is doing.
In the event of the patient having several fits, one after the other, it may be necessary to give him an anti-epileptic drug such as Diazepam. SEEK URGENT RADIO MEDICAL ADVICE.
Shock and circulatory collapse
Shock occurs when the body's circulatory system is unable to distribute oxygen enriched blood to all parts of the body. If untreated, the body's vital organs (brain, heart, lungs, kidneys) can fail, leading to collapse, unconsciousness and eventually death.
Causes
The commonest cause is loss of body fluid from the circulation. It can result, either from external or internal bleeding, (e.g. as occurs in fractures of the thigh), the formation of large blisters and the weeping of fluid from large burns and from damaged blood vessels in crush injuries. Shock can also be found in severe heart attacks, and in certain diseases characterised by excessive vomiting and diarrhoea.
The first-aider should always be on the look-out for this condition as it can develop even while the casualty is under close observation and it may be missed. Fear, pain and exposure to cold make shock worse.
Symptoms and signs
The patient:- will usually lie still, taking little notice of his surroundings
- will complain of feeling faint, cold and thirsty. He may shiver;
- his lips and the edges of the ears may be blue;
- his skin will be pale, cold and clammy;
- his pulse will be rapid and weak;
- his respiration will be rapid and shallow and, as shock deepens, he will give frequent sighs;
- he may start to vomit;
- if untreated, he may lapse into unconsciousness and later die.
Treatment
The primary aim is to treat whatever condition is causing the shock;- lay the patient flat and, if injuries permit, elevate the feet and legs so that blood flows to the heart and brain (see note below on exceptions to this rule);
- do not move him unless in a position of danger;
- stop any blood loss. Cover burns and scalds. Immobilise fractures.
- loosen any tight clothing which restricts breathing movement;
- keep warm but do not overheat.
- deal with any pain. Morphine may be given as necessary
- give small sips of water if there is no suspicion of abdominal injury but NEVER give fluids to an unconscious casualty. A badly burned or scalded person may require much more fluid;
- move to a place of safety as gently as possible. Rough handling will increase the pain and the shock.
Exceptions to the lay flat rule:
- position with the head turned with the damaged side underneath and, if possible, with a head-down tilt. This will prevent blood running down into the throat and lungs;
- if there is a penetrating wound of the chest, or if breathing is difficult, prop up to assist breathing;
- if unconsciousness occurs, put into the unconscious position with as little disturbance as possible to the injured part.
Bleeding
External bleeding
Bleeding from small blood vessels occurs when there is a minor cut or abrasion of the skin. Blood oozes from the wound; it usually stops by itself or when a dressing is applied. It is generally of no consequence.
In large and deep wounds, the blood wells up in a steady stream. The volume of blood loss depends on the number of blood vessels damaged and, although it may appear alarming, it is not usually dangerous, unless allowed to continue.
When large arteries are damaged, bright red blood will spurt from the wound in time with the heart beats. This bleeding is usually profuse and the patient's life will be endangered. This is a rare situation.
In all cases of external bleeding, follow the three cardinal rules:- lay the patient down;
- lift up the affected part if possible;
- press firmly where the blood comes from. Use a dressing or a clean cloth or handkerchief but, if none should be available, use the bare hand or fingers. When possible disposable gloves should be worn to protect yourself.
This procedure will stop the flow of blood.
When bleeding has been controlled, apply a standard dressing to the wound and bandage firmly and widely in position. There may be a slight staining of blood through the dressing, which is of little consequence, but if blood soaks quickly through the pad it is a sign that the bleeding has not been properly controlled. If this happens, do not disturb the dressing, but put another standard dressing on top and bandage more firmly. This will usually stop the bleeding. Very occasionally, a third dressing may be required.
Do not disturb the dressings until you are prepared to undertake definitive treatment. The bleeding stops because of the formation of a clot. If you remove the dressing, the clot will break and bleeding will start again.
Special types of external bleeding
From an open fracture
The bleeding comes mainly from around the break and not from the bone.
- do not attempt to elevate the part, this will cause further pain and damage;
- apply a dressing, sterile if possible, padding around the wound. Firm bandaging will apply the necessary pressure to the tissue around the exposed bone ends.
From a tooth socket:
- The socket may bleed after the extraction of a tooth. This kind of bleeding is seldom serious. At least two-thirds of the 'blood' which is spat out will be saliva, so the blood loss is unlikely to be great;
- if the gum margins are splayed out, squeeze them gently together to close up the tooth socket;
- fold a piece of gauze tightly and place it in the socket so that it is standing proud of the level of the remaining teeth;
- the casualty should close his mouth, biting firmly on the gauze in the tooth socket. The pressure should be maintained for 20 minutes. If the socket is still bleeding on removing the gauze pad, the procedure should be repeated as often as is necessary (Figure 1.36).
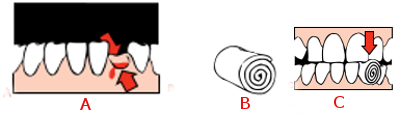
Figure 1.36
From the ear passage:
- This is usually caused by a head injury or by blast:
- place a large pad over the ear and bandage it in position;
- keep the affected ear downwards;
- if the casualty is unconscious, place in the unconscious position with the affected ear downwards;
- never plug the ear passage with cotton wool or other material.
From the nose:
- the casualty should sit with his head over a basin or bowl while pinching the soft part of his nose firmly for 10 minutes; (Figure 1.37);
- he should then release the pressure slowly;
- if bleeding has not stopped, he should repeat the manoeuvre for a further 10 minutes;
- it might be necessary to do this for a third time;
- if bleeding has not stopped after half-an-hour, it might then be necessary to pack the nose with ribbon gauze. See Chapter
The care and treatment, after first-aid

Figure 1.37
From the lips, cheek and tongue:
- press on both sides of the lip, cheek or tongue to stop bleeding;
- use a piece of gauze or a swab on each side to help maintain pressure and stop the fingers slipping (Figure 1.38);
- pressing is usually most easily done by the casualty with direction from another person, or helped by looking in a mirror.

Figure 1.38
Internal bleeding
Internal bleeding may be caused by injury, disease, or by the action of certain poisons. Any severe injury to the body will cause bleeding of varying degree. Bleeding may be limited to the soft tissues, such as muscles, but when a bone breaks there is always bleeding at the fracture site. Minor injury will affect only the superficial tissues and the bleeding may be limited to small amounts which will appear as bruising. Greater force will result, in addition to bruising, in the formation of a collection of blood within the deeper tissues (a haematoma). This causes painful swelling of the affected part and may be difficult to distinguish from a fracture. Whatever the nature of such injuries, the blood loss very rarely endangers life.
In contrast, bleeding from injury to internal organs is always very serious and may quickly endanger life. Such bleeding is always concealed and its presence has to be deduced from the history of the injury, a rising pulse rate and the signs and symptoms of shock which occur rapidly. The abdominal organs are poorly protected by the abdominal wall and they are particularly liable to injury by direct or crushing forces. These internal injuries require expert treatment urgently and every effort must be made to deliver the casualty to medical care. Always get RADIO MEDICAL ADVICE. There is little that can be done aboard because a blood transfusion may be needed.
If internal bleeding is suspected:- put in bed with a head-down tilt;
- if conscious and in pain or restless, give morphine 10 mg;
- cover with only one blanket;
- record the pulse rate at 10 minute intervals. A falling rate may indicate that the bleeding has stopped (Figure A);
- give fluid per rectum ;
- if the injury is abdominal, allow the patient to suck flakes of ice. With bleeding from other parts of the body, sips of water may be given;
- treat for shock.
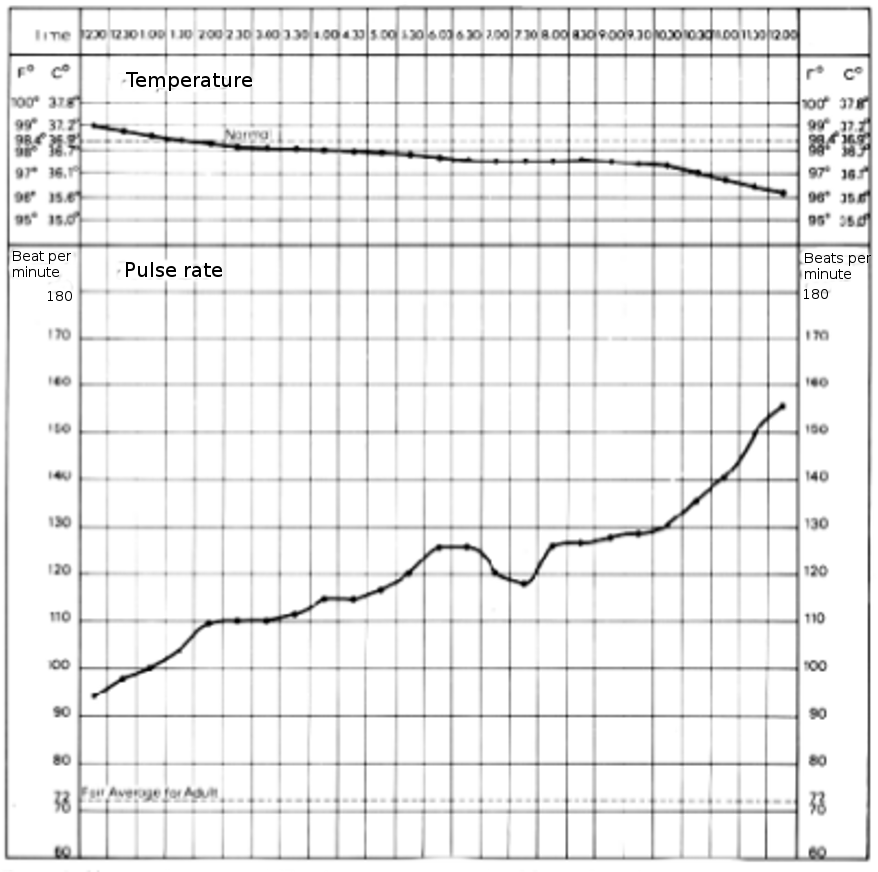
haemorrhage - falling temperature and the rising pulse rate
Figure A
Coughing up or vomiting blood
NOTE: remember that bleeding can occur from the back of the nose, a tooth socket, bleeding gums, etc. It is important that this should not be confused with bleeding from the stomach or lungs.
Coughing up of blood
In some lung diseases and cases of injury to the chest, blood may be coughed up. Except in cases of injury this is seldom fatal.
Treatment is the same as for internal bleeding with the exception that the patient should be placed at rest with the head and shoulders raised. It is not usually necessary to give fluid per rectum. For further care see Chapter The care and treatment, after first-aid
See Examination of sputum .
Vomiting blood
Blood may be vomited if the stomach is injured by a wound of the abdomen or if blood collects in the stomach as a result of a bleeding peptic ulcer. In the latter case the patient may suddenly vomit a quantity of dark brown fluid like coffee grounds. He feels faint and looks pale. If the bleeding and vomiting continue he will suffer increasingly from shock.
Treatment is the same as for internal bleeding. For further treatment of this condition. If there is a wound of the abdomen, this should be treated.
Wounds
A wound at any site in the body poses three problems:- control of bleeding;
- prevention of shock
- prevention of infection There are some simple rules:
- never wash the wound – except in cases of an animal bite
- never try to remove pieces of metal or glass from a wound unless they are superficial and can be easily lifted out. If pieces can be removed, do it by grasping the material with sterile gauze or use sterile forceps, if available;
- do not pour antiseptic into a wound;
- as soon as possible, cover the wound with a suitable dressing.
Bullet or metal fragment wounds
In this type of injury, look for and treat any exit wound. This is usually larger than the entry wound. Remember that there may be underlying bone fractures and that the bullet or metal fragment may have been deflected from the bone to cause serious internal damage, the only signs of which may be increasing shock.
Chest wounds
A superficial chest wound should be treated as for any wound elsewhere but a penetrating wound (a sucking wound) of the chest must be sealed immediately, otherwise air is drawn into the chest cavity and the lungs cannot inflate as the vacuum inside the chest is destroyed. A useful dressing for a sucking wound can be made from a paraffin gauze dressing. Place the paraffin gauze over the wound, smooth the foil on to the chest wall and seal three edges only with zinc oxide adhesive plaster. In emergency, a suitable dressing may be improvised from petroleum jelly, gauze and kitchen foil or polythene or, alternatively, a wet dressing may be used to provide an airtight seal. If nothing else is available, use the casualty’s own bloodstained clothing to plug the wound temporarily. The aim is to prevent air entering the chest but to allow it to escape if necessary.
The usual rules about stopping bleeding by pressing where the blood comes from also apply. Start a pulse chart soon to check on possible internal bleeding in all chest injuries. The respiratory rate should also be recorded. See also sections on chest injuries.
Conscious casualties should be placed in the half-sitting-up position because breathing is easier in this position.
NOTE: DO NOT GIVE MORPHINE to a patient with this type of wound, even if he is suffering from a lot of pain, as the morphine will increase the breathing difficulties. Get RADIO MEDICAL ADVICE.
Abdominal wounds
A superficial abdominal wound will require the same treatment as any wound, but for more serious wounds, if the abdominal contents do not protrude, cover the wound with a large standard dressing and place the casualty in the half-sitting-up position (Figure 1.39). In this position the wound will not gape open. As the abdominal muscles are slack, the abdominal contents will not bulge through. If the wound runs more or less vertically, it may be best to lay the man flat.

Figure 1.39
If the abdominal contents do protrude through the wound, DO NOT ATTEMPT TO PUT THEM BACK. Cover with a loosely applied large standard dressing or dressings until further treatment can be given. Shock will develop quickly and should be treated as described previously, with the following important exceptions:
- prop up if necessary;
- DO NOT give anything by mouth. If thirsty, the lips should be moistened; nothing more. (See also Crush wounds and Stab wounds below).
- Get RADIO MEDICAL ADVICE.
Head wounds
The wound itself should be treated in the same way as any other wound. Scalp wounds often bleed briskly. A firm bandage will usually arrest the bleeding, but some ingenuity may be required in applying the bandage so as to keep it firmly on the head and transmit the necessary pressure to the pad. Firm pressure by the fingers over the pad for a few minutes before it is finally fixed in position will help to stop the bleeding.
The possibility of brain damage is of greater importance and two rules should be observed:- morphine should be given only if conscious and in much pain from more serious injuries elsewhere;
- if unconscious, put in the unconscious position and give the treatment described in Chapter The care and treatment, after first-aid
- Get RADIO MEDICAL ADVICE.
Face and jaw wounds
There may be danger of suffocation as a result of blood running into the throat. Lay flat in the unconscious position (Figure 1.26) with the more damaged side underneath. If the casualty is to be removed by stretcher, see that he remains in that position. With severe wounds there may be loss of the power of speech. Give reassurance; speech will probably return to normal when healing has taken place.
Palm of the hand wounds
A deep wound of the palm of the hand may cut the large artery in this area. If this occurs:- stop the bleeding by pressing where the blood comes from;
- cover the wound with a sterile gauze dressing and ask the patient to grasp firmly on a rolled-up 7.5 cm bandage;
- a hand bandage, firmly applied, will hold the dressing in place and will maintain the pressure necessary to control the bleeding.
Crush injuries
Limbs
After a crush injury, at first there may be very little to see. However, considerable damage may have been done to the muscles and other soft tissues and gross swelling may take place later. Shock, which may be very severe, may also develop.
- treat any wound;
- the affected limb should be immobilised and supported in its most comfortable position;
- treat shock as described but:
- do not give large amounts of fluid at once as the casualty will vomit;
- give frequent small amounts of water only.
- GET RADIO MEDICAL ADVICE.
Chest
Crushing of the chest may stop breathing and then artificial respiration will be required. If ribs have been fractured, treat as described under fractures.
See also section on chest injuries.
Abdomen
Severe crushing of the abdomen may cause rupture of the internal organs and/or internal bleeding. If you suspect that this has occurred, Get RADIO MEDICAL ADVICE. See general advice on abdominal wounds at beginning of this section and stab wounds below.
Stab wounds
Stab wounds are especially dangerous because the underlying structures will have been penetrated and infection will have been carried into the deep tissues.
Chest:
- if the lung has been penetrated, it will collapse giving rise to breathlessness and coughing of bright red frothy blood;
- a sucking wound can be created;
- the heart can be damaged.
- Get RADIO MEDICAL ADVICE
- see also section on chest injuries.
Abdomen
Depending on the position of the wound (see Anatomy Diagrams, Annex II), an organ may be pierced, giving rise to peritonitis and internal bleeding. See general advice at beginning of this section. Get RADIO MEDICAL ADVICE.
Limbs
Muscles, nerves and blood vessels may be cut. Bleeding, both internal and external, will occur. Whatever the site of the stab wound, the immediate treatment is the same:
- stop external bleeding by pressure
- prevent further infection by applying suitable dressings
- treat shock if necessary.
Fractures
A fracture is a broken bone. The bone may be broken into two or more pieces with separation of the fragments or it may have one or more fissured cracks without any separation.
Most fractures are caused by direct force, but force may be transmitted through the body to cause injury indirectly elsewhere. Two classical examples are: a fall on the outstretched hand, causing a fracture of the collar bone; and a fall from a height on to the heels, causing a fracture of the base of the skull.
A much less common type is a stress fracture. The bone becomes weakened in a way comparable to metal fatigue. Sudden, strong muscular effort may snap the bone.
In simple terms, a fracture may be open to infection or closed to infection.
A closed fracture
There is no communication between the fracture and the surface of the body.
An open fracture
There is communication between a skin wound and the fracture. Open fractures are always serious because germs may enter through the wound to cause infection of the broken bone and the surrounding tissues.
NOTE: A skin wound may be present but, unless it is deep enough to reach the broken bone, the fracture is still closed. Open or closed fractures are sometimes complicated by damage to important structures such as the brain, lung, blood vessels or nerves.
Principles of treatment
It is not possible to set fractures on board ship. Indeed, many fractures may not require setting and unskilled attempts might prejudice healing. First aid measures should ensure adequate immobilisation. Wherever a fracture case has to be kept on board for more than two or three days, the joints above and below the fracture site should be gently put through a full range of movements, morning and night.
Lasting damage may result if a joint surface is involved in the fracture and in all cases where this is suspected, RADIO MEDICAL ADVICE must be sought.
Antibiotic treatment must always be given as soon as an open fracture is diagnosed or suspected.
Examination
The following signs and symptoms will indicate that the bone is probably broken:- a heavy blow or other force has been applied to the body or limbs. The casualty or others may have heard the bone break;
- intense pain, especially on pressure or movement at the site;
- swelling. The site may be swollen and/or bruised. This may be due to internal bleeding;
- loss of use. The casualty may be unable or unwilling to use the injured part because of the pain. He may also experience severe pain if an attempt, even very gently, is made to help him make the movement. Watch his face for signs of pain. Occasionally, if the broken ends of a bone are impacted together, the person may be able to use the part but usually only with a fair amount of pain;
- distortion. Compare good and bad limbs or sides of the body to see if the part is swollen, bent, twisted or shortened;
- irregularity. The irregular edges of a broken bone can sometimes be seen in an open fracture. They may be seen or felt under the skin in a closed fracture;
- unnatural movement and grating of bone ends. Neither of these symptoms should be sought deliberately. A limb may feel limp and wobbly and grating may be felt when trying to apply support to the limb. In either of these situations, the bone is certainly broken.
General treatment
- bleeding should be treated as described;
- rest the affected part by immobilisation. This prevents further damage, relieves pain and stops further bleeding;
- all fractures or suspected fractures must be immobilised before making any attempt to move the casualty. This can be done using wooden, improvised or inflatable splints, or by fixing a limb to the body, or – in the case of the legs – by lashing one to the other.
Immobilise a limb in the position in which it is found, if it is comfortable. If it does become necessary to move an injured limb, because of poor circulation or for any other reason, first apply traction by pulling the limb gently and firmly away from the body before attempting to move it (Figure 1.40).
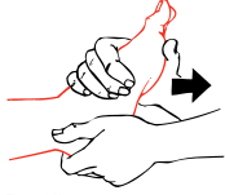
Figure 1.40
Keep pulling until it has been securely immobilised and then release the traction very slowly. Sudden release can cause pain.
Circulation of the blood in a fractured limb. Check that the circulation to the limb is intact. To do this, press on the nail of the thumb or of the big toe. When circulation is normal the nail becomes white when pressed and pink when released. Continue checking until you are satisfied that all is well. Danger signs are:
- blueness or whiteness of fingers and toes;
- coldness of the parts below the fracture;
- loss of feeling below the injury. Test for this by touching lightly on fingers and toes and asking the casualty if he can feel anything;
- absence of pulse.
If there is any doubt at all about the circulation, loosen all tight and limb-encircling dressings at once and straighten out the limb, remembering to use traction when doing so. Check circulation again. If the limb does not become pink and warm and you cannot detect a pulse, then medical help is urgently necessary if amputation is to be avoided. Get RADIO MEDICAL ADVICE.
- remember that fractures can cause severe internal bleeding ;
- always look for and treat for shock;
- morphine may be necessary to control pain.
Collar bone, shoulder blade and shoulder
Fractures in these areas are often the result either of a fall on the outstretched hand or a fall on to the shoulder. Direct violence to the parts is a less common cause of these fractures.
Place loose padding about the size of a fist into the armpit. Support the arm using a triangular sling (Figure 1.41). Then tie the arm to the body, using a narrow fold bandage. Keep the casualty sitting up as he will probably be most comfortable in this position.

Figure 1.41
Upper arm
Upper arm fractures are usually caused by direct violence. Bind the upper arm to the body, using a broad fold bandage. Bend the elbow gently and apply a collar and cuff sling (Figure 1.42). Keep the casualty sitting up so that the weight of the arm can supply traction to the lower fragment. Alternatively, upper arm fractures may be splinted. Bend the elbow gently. Use three well padded splints. Place one behind the upper arm, one in front and the third from the tip of the shoulder to the elbow. Bandage the splints securely in place. Support the arm with a collar and cuff sling (see also Figure 1.21).
Figure 1.42
Elbow
Fractures in this area can be especially dangerous because of damage to blood vessels and nerves around the elbow. Check circulation and feeling in the fingers. If the finger tips are white or blue and feeling is absent or altered, the elbow must be straightened at once. Tell the casualty to lie down. Be gentle. Apply traction on the hand and forearm. Bring the arm and forearm slowly and carefully to the casualty's side. Now place plenty of loose padding between the arm and the body and also around the arm. Then bind the forearm to the body by encircling ties. Check the circulation again when you have made the encircling ties. If the circulation is poor, the ties should be loosely secured until the casualty has to be moved (Figure 1.43).
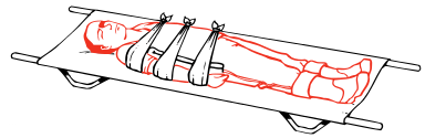
Figure 1.43
Forearm and wrist
Fractures in this area commonly result from a fall on the outstretched hand. Bend the elbow until the forearm is across the body. Then apply an arm sling (Figure 1.20). Remove any finger rings. Later, apply two well padded splints to the back and front of the forearm and secure firmly, using narrow fold bandages. Support the arm with a broad arm sling. For fractures of the wrist bones, put a broad, well padded splint on the front of the forearm and the palm of the hand. Put plenty of padding on the back of the forearm and hand and secure. Use a broad arm sling for support.
Hand and fingers
Fractures of the hand bones (metacarpals) and the finger bones are a common result of shipboard accidents and expert treatment may be many days away. As fixation in a straight splint is only permissible for a short time, the treatment described in the following paragraphs should be undertaken if the casualty has to be kept on board. Always remove rings immediately.
The hand bones (metacarpals):
- apply a crepe bandage around the hand and wrist firmly enough to support the injured part but not so tight as to prevent movement of the wrist and finger joints;
- check that circulation to the fingers is present;
- elevate the hand by placing the arm in a triangular sling to reduce the swelling;
- encourage the casualty to move the wrist and all the finger joints frequently.
The fingers:
- strap the finger to the adjacent finger, using zinc oxide adhesive plaster (as shown in Figure 1.44);
- be careful that you do not prevent movement of the finger joints. Do not put the plaster directly over the fracture;
- to avoid swelling, elevate the hand by putting the arm in a triangular sling;
- encourage the casualty to move all the finger joints.

Figure 1.44
Open fracture of the fingers:
- stop the bleeding and apply a dressing to the wound;
- if the dressing prevents strapping to the adjacent finger, use as a splint, a strip of aluminium or other soft metal 2 cm wide and long enough to stretch from the tip of the finger to just below the wrist joint;
- immobilise the finger in the position shown in Figure 1.45. This is done by bending the splint to conform with the joints, using the same finger of the undamaged hand as a pattern, and taking care to ensure that the splint will not dig into the back of the hand or into the wrist;
- pad the splint with two layers of elastic adhesive bandage along its length. Turn the bandage over the ends to protect the skin;
- fix the splint to the finger with zinc oxide plaster cut to suitable widths;
- give standard antibiotic treatment

Figure 1.45
Crush injuries to the hand
Severe crushing injuries to the hands may cause multiple open or closed fractures of the metacarpal or finger bones. Other wounds are likely to be present.
- stop the bleeding and apply dressings;
- pain will be severe. Give analgesics (Morphine if necessary);
- if hospital treatment is not available quickly, read the section on definitive treatment of wounds and treat accordingly.
Hip to knee
A broken thigh bone is a potentially serious injury. It causes significant internal bleeding into the muscles of the thigh and, with the associated pain, shock very quickly develops. If it is combined with other serious injuries, the blood loss may be so great as to require blood replacement. Get RADIO MEDICAL ADVICE.
- a break of the neck of the thigh bone causes shortening of the injured leg and the casualty will lie with the whole lower limb and foot flopped outwards. There will be severe pain in the region of the hip;
- fractures of the shaft of the thigh bone exhibit the usual signs and symptoms of a fracture. Severe pain is a normal feature. If you think that the thigh is broken:
- first, pad between the thighs, knees, calves and ankles, using folded blankets or any other suitable soft material;
- bring the good leg to the broken leg. Do this slowly and carefully;
- bring the feet together. If attempting to do this causes pain, apply traction to the injured leg gently and slowly, and then try again;
- tie encircling bandages: around both feet; halfway between the knees and the ankles; just above the knees; and at the upper thighs. Avoid making any ties over the site of the fracture (Figure 1.46);
- the shoe on the affected side can now be removed so that you can check the circulation in the toes – if necessary, loosen any bandages – and then replace the figure-of-eight bandage around the ankles and feet;
- treat for shock and pain – morphine will be needed.

Figure 1.46
Kneecap
This fracture may be caused by direct violence or as a result of a sudden stress on the bone. It is commonly a closed fracture. When an open fracture occurs, the wound should be treated before splinting is undertaken and antibiotic treatment should be given.
- place the casualty in a half-sitting-up position and put supports behind his back to maintain this. Raise the leg and hold it in a comfortable position.
- choose a splint long enough to reach from the buttock to beyond the heel, pad it well and apply it along the back of the leg. Put additional padding behind the hollow at the heel so as to lift it off the splint, and also behind the knee;
- secure the splint in place with bandages round the thigh, round the lower leg just below the knee and with a figure-of-eight bandage at the ankle, and elevate the leg on a suitable support (Figure 1.47).
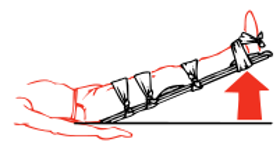
Figure 1.47
When the casualty is moved to the cabin or to the ship's hospital, he should be kept in a sitting position with the leg elevated.
When medical attention will not be available for some time and it is obvious that there is a wide gap between the fragments of the knee cap, carry out the procedure described above, but put a figure-of-eight bandage round the knee, beginning above the knee cap and finishing over padding applied just below it (Figure 1.48).
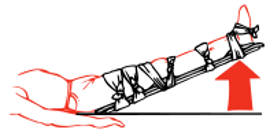
Figure 1.48
This method will draw the fragments together and hold them in place. Check that the circulation is intact.
Knee to foot
Lower limb
These should be treated in the same way as fractures of the thigh. See also below for fractures of both legs.
Ankle
An ankle fracture which is stable and without any deformity can be given adequate but temporary first aid by placing the injured ankle on a number of pillows to keep it at rest (Figure 1.49).

Figure 1.49
In more serious fractures of the ankle it is usual to find a good deal of deformity and swelling, and splinting may be necessary.
- remove the casualty's shoe and sock;
- obtain two splints, long enough to stretch from just below the knee to the sole of the foot. Pad these well to allow for the deformity and swelling, and apply them to both sides of the leg;
- fix them in place with a figure-of-eight bandage to the foot and place other bandages just below the knee and above the ankle;
- check that the circulation is intact.
Heel bone
These fractures usually occur when the casualty has fallen from a height and lands on his heels. As force has been transmitted upwards, there may be more serious fractures elsewhere, e.g. spine and base of the skull, and the patient should be carefully examined to exclude these.Treat as above, for fractures of the ankle.
Bones of the foot
Severe injuries are usually the result of heavy weights being dropped on to unprotected feet or of crushing. Fractures of the toes may occur when they are stubbed against some hard object.
- remove the boot or shoe and the socks carefully;
- treat any wound.
- keep the foot elevated and use pillows to keep it in a comfortable position.
Both legs
As there is no good leg to act as a splint for the other, external splinting will have to be used. There may be considerable blood loss if both legs are broken.
- have well padded splints available. These should reach from the thigh to the ankles on the outside of both the legs for below the knee fractures, and from the armpit to the ankles for above the knee fractures;
- pad between the thighs, knees, calves and ankles;
- bring both feet together as gently as you can, using traction if necessary.
- tie a figure-of-eight bandage round the feet and ankles to keep the feet together;
- apply the padded splints to the outside of both legs;
- tie enough encircling bandages to keep the splints and the legs secured firmly together. Avoid making any ties over the site of any break (Figure 1.50);
- check the circulation in both feet as described for thigh fractures;
- move the casualty in a Neil Robertson stretcher.
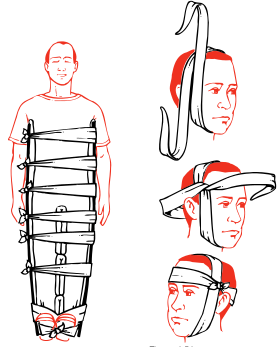
Figure 1.50 Figure 1.51
Jaw
Normally, fractures of the lower jaw give little trouble.
- casualty sits with the teeth clenched, often refusing to speak much on account of the pain;
- the spasm of the jaw muscles caused by pain keeps the teeth clenched and jaw immobilised;
- a bandage, tied as in Figure 1.51, will support the lower jaw. A major hazard arises when both sides of the lower jaw are fractured. In this case, the jaw with the tongue attached on the inside of it, can move backwards and may obstruct the air passage.
- hook a finger, yours or the casualty's, over and behind the lower front teeth and pull the jaw, and with it the tongue, forwards;
- if possible, arrange for the casualty to sit up with his head forwards;
- if he cannot sit up, on account of other injuries, place him in the unconscious position and someone must stay with him, keeping the jaw pulled forward, if necessary, and watching carefully for any sign of obstructed breathing.
Spine
Always suspect a fracture of the spine if a person has fallen a distance of over two metres. Check carefully how the injury happened. Ask if there is pain in the back. Most people with fractures of the spine have pain but a very few DO NOT. If in doubt, treat the injury as a fractured spine.
A FRACTURED SPINE IS POTENTIALLY A VERY SERIOUS INJURY. IF YOU SUSPECT A FRACTURED SPINE, TELL THE CASUALTY TO LIE STILL AND DO NOT ALLOW ANYONE TO MOVE HIM UNTIL FIRST AID TREATMENT HAS BEEN COMPLETED.
Any careless movement of a casualty with a fractured spine could damage or sever the spinal cord, resulting in permanent paralysis and loss of feeling in the legs, and double incontinence for life. He can, however, be safely rolled over onto one side or the other because, if this is done very gently and carefully, there is very little movement of the spine.
First, establish whether the spinal cord has been damaged. To do this:
- ask the casualty if he can feel any tingling of the feet or legs. Tingling usually means that there is some pressure on the spinal cord;
- ask him to move his toes. If he is unable to do this, then paralysis is present and indicates severe damage to the spinal cord;
- run your fingers lightly over the skin of the lower legs and feet. Absence of sensation indicates severe damage to the spinal cord.
If any of these are found, get RADIO MEDICAL ADVICE.
- next, place padding between the legs;
- tie the feet and ankles together with a figure-of-eight bandage and get the casualty lying still and straight. Use gentle traction on the head and on the feet to straighten him out. Do not bend him. Take your time;
- tie a narrow fold bandage around the casualty at the level of his elbows and mid thighs. This method keeps the casualty rigid (Figure 1.53);
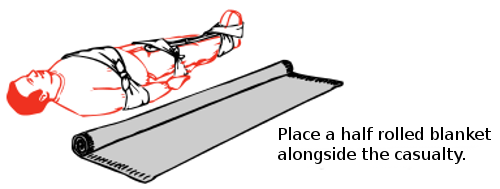
Figure 1.53
- place pads to fill and support the hollows of the spine at the small of the back and at the neck (Figure 1.52);

Figure 1.52
- he can now lie safely in this position for as long as is necessary. So do not be in a hurry to move him;
- prepare a stiff supporting stretcher ready for the patient. There may be a need to stiffen the Neil Robertson stretcher with broom handles. A canvas stretcher will not do unless it has stiff wooden boards laid transversely over the canvas to provide a rigid support for the back. Two pads must be provided to support and fill the hollows of the spine in the small of the back and behind the neck. The back pad should be larger than the neck pad (Figure 1.52);
- when the stretcher has been prepared and is alongside the casualty, the next job is to lift him onto the prepared stretcher as described in Figures 1.53 to
1.58;
NOTE: In Figures 1.54 to 1.58 the encircling bandages shown in Figure 1.53 round the thighs and at the elbows have been omitted for clarity. See also Notes at end of this Section; - to lift the casualty, have at least two people grasping each side of the blanket and one person at the head and one at the feet to provide in line support. Those lifting the blanket should be spaced so that more lifting power is available at the body end, which is heavy compared to the legs. A further person is required to push the prepared stretcher under the casualty when he is lifted (Figure 1.57);
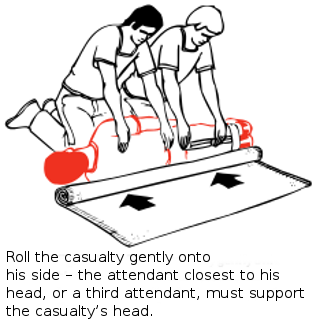
Figure 1.54
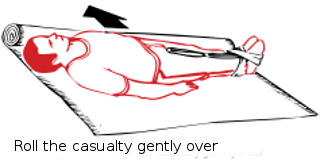
Figure 1.55
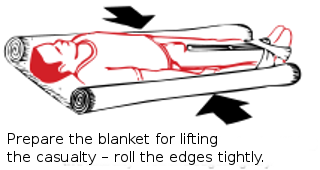
Figure 1.56
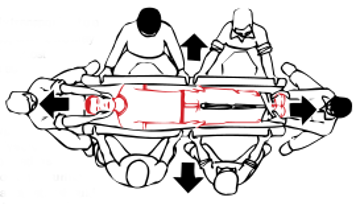
Figure 1.57
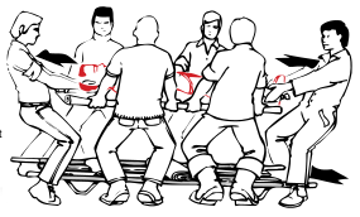
Figure 1.58
- lift the casualty very slowly and carefully to a height of about half a metre. The height should be just enough to slip the stretcher under the casualty. Be careful, take time, keep the casualty straight (Figure 1.58);
- slide the stretcher between the legs of the person who is supporting theankles. Then move the stretcher towards the head end until it is exactly underneath the casualty. Adjust the position of the pads to fit exactly under the curves in the small of the back and neck;
- lower the casualty very, very slowly on to the stretcher. Maintain support until he is resting firmly on the stretcher (Figure 1.58);
- the casualty is now ready for removal.
When the casualty has been very carefully transported to a mattress on the deck, or other very firm bed, where he may remain undisturbed flat on his back, the most important single point is to keep him as still as possible. He must continue to be supported with pillows, etc., as described later in the text. Every care and attention, and encouragement must be given to help him to remain still, whether or not any paralysis is present. Bags filled with sand should be placed as necessary to prevent the body or limbs rolling. A urine bottle should be constantly available, and a catheter should be used to relieve him if necessary. He should pass any faeces on to cotton wool or other material: he must not be lifted on to a bed pan. His back should be treated, so far as possible, to prevent sores. He must be put ashore at the very earliest possible moment. Get RADIO MEDICAL ADVICE.
NOTES:
(1) As there are a number of people helping and since it is important to take great care in handling the casualty, it may be helpful to have a person read
out the particular instruction before each operation is carried out.
(2) At least seven people are required to carry out this manoeuvre. In ships with small crews, there may be insufficient numbers of men available. In this case,
do not attempt to move the casualty but carry out the instructions given above on immobilising him and padding the natural curves of the spine. The casualty should
then be kept warm, his pain should be treated (see section on analgesics and, if he is on the deck, he should be protected from the elements with suitable
waterproof coverings
Neck
Injuries to the neck are often compression fractures of the vertebrae due, for example, to a person standing up suddenly and bumping his head violently, or by something falling on his head. Falls from a height can also produce neck injuries. Treatment is similar to that described above for fractures of the spine, because the neck is the upper part of the spine.
- the casualty should be laid flat, if not already in this position, and should be kept still and straight;
- a semi-rigid neck collar should then be applied gently to stop movement of the neck while an assistant steadies the head. An improvised neck collar can be made quite easily from a newspaper. Fold the newspaper so that the width is about 10 cm at the front. Fold the bottom edge over to produce a slightly narrower back. Then fold this around the neck with the top edge under the chin and the bottom edge over the top of the collar bones;
- tie a bandage, scarf or a necktie over the newspaper to hold it in place. This will keep the neck still (Figure 1.59).

Figure 1.59
Chest
See Fractured ribs.
Pelvis
A fracture of the pelvis will result from direct violence in the pelvic area or from a fall from a height when the casualty has landed on both feet with the legs held stiffly. The main danger of this injury is of damage to the pelvic organs, especially the bladder and the urethra (the pipe which leads from the bladder to the tip of the penis).
- the casualty will complain of pain in the hip, groin and pelvic areas and, perhaps, also of pain in the lower back and buttock areas, made worse by moving or coughing;
- he will be unable to stand, despite there being no injury to the legs;
- he may want to pass urine although he may be unable to do so. If urine is passed, it may be blood-stained.
- there may be signs of internal bleeding;
- the compression test is useful. Press gently on the front of both hip bones in a downward and inward direction so as to compress the pelvis. This will give rise to sharp pain if it is broken. Some movement of the pelvic bones may also be felt if there is a fracture (Figure 1.60), but do not continue pressing in an attempt to elicit this sign, as further damage may be caused.

Figure 1.60
If you think that the pelvis may be fractured, tell the casualty:
- not to move;
- not to pass any urine if he can avoid it. If urine is passed, look for staining with blood.
Remember that: - if the bladder or urethra is damaged, urine can leak into the tissues;
- bleeding into the surrounding tissues and into the pelvic and lower abdominal cavities may be severe. A pulse chart must be started immediately to check for internal haemorrhage.
- lay the patient in his most comfortable position. This will usually be on his back. If he wants to bend the knees, support them with pillows. Place padding between the legs;
- apply a broad fold bandage round both knees and a figure-of-eight bandage around the ankles;
- move the casualty with great care. Use the same technique as for fracture of the spine.
- keep checking for internal bleeding.
- when moved to a cabin or to the ship's hospital, allow the casualty to lie in whatever position he finds most comfortable;
- morphine may be required to control the pain;
RADIO MEDICAL ADVICE should be obtained.
Dislocations
A dislocation is present when a bone has been displaced from its normal position at a joint (Figure 1.61). It may be diagnosed:
- when an injury occurs at or near a joint and the joint cannot be used normally;
- movement is limited or impossible;
- there is pain, often quite severe. The pain is made worse by attempts to move the joint;
- the area is misshapen both by the dislocation and by swelling (bleeding) which occurs around the dislocation;
- with the exception of no grating of bone ends, the evidence for a dislocation is very similar to that of a fracture;
- always remember that fractures and dislocations can occur together.
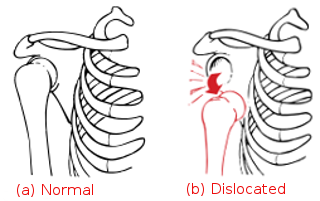
Figure 1.61
Treatment
- dislocations can be closed or open. If a wound is present, at or near the dislocation, the wound should be covered, both to stop bleeding and to help to prevent infection; give antibiotic treatment;
- do not attempt to reduce a dislocation. A fracture may also be present and attempted manipulation to reduce the dislocation in these circumstances can make matters worse;
- prevent movement in the affected area by suitable immobilisation. The techniques for immobilisation are exactly the same as for fractures of the same area(s).
- look out for impaired circulation and loss of feeling. If these are present, and if you cannot feel a pulse at the wrist or ankle, try to move the limb gently into a position in which circulation can return and keep the limb in this position. Look then for a change of the fingers or toes, from white or blue to pink;
- transport the casualty in the most comfortable position. This is usually sitting up for upper limb injuries and lying down for lower limb injuries;
- for further treatment of dislocations of the shoulder and of the fingers, see in Chapter The care and treatment, after first-aid
Head injuries
Head injuries commonly result from blows to the head and from falls, often from a height.
Most preventable serious head injury deaths result from obstructed breathing and from breathing difficulties, not from brain damage. Apart from covering serious head wounds, your attention should be concentrated on the life-saving measures which support normal breathing and which prevent obstructed breathing. This will ensure that the brain gets sufficient oxygen easily. In this way you have a good chance of keeping the casualty alive in order to get him skilled medical aid in a hospital; get RADIO MEDICAL ADVICE.
NOTE: in the case of some head injuries or where a foreign body or a fracture is directly below an open wound, you should NOT control bleeding by direct pressure on top of the wound. In these circumstances a sterile gauze dressing is applied over the wound and a bandage is padded around the wound and over the edge of the dressing, held firmly in place by a bandage. see Chapter The care and treatment, after first-aid for further information.
Chest injuries
See also Wounds, Crush wounds, Stab wounds.
Fracture of the ribs
This is a common fracture which is usually caused by falling against a hard surface or by a crushing injury. Signs and symptoms are:
- sharp, continuous pain which is increased when breathing in or by coughing;
- shallow breathing to prevent chest movements;
- marked localised tenderness when the injured area is felt gently.
Uncomplicated rib fracture:
- make the casualty sit down in the normal sitting position but, if pain is severe, place him in the half-sitting-up position, leaning over towards the injured side;
- transport him in this position to the ship’s hospital or his cabin;
- treat pain;
- do not put strapping around his chest;
- keep him at rest in the position he finds most comfortable, either in bed or sitting in a chair or on the floor (Figures 1.62, 1.63, 1.64).

Figures 1.62

Figures 1.63

Figures 1.64
Severe chest injuries
The ribs form a rigid cage which protects the heart and lungs. Severe force may cause any one or a combination of the following injuries:
- a superficial wound and/or bruising of the chest
- a penetrating (sucking) wound of the chest wall
- multiple rib fractures on one or both sides of the chest, together with injury to the underlying lung and its covering (the pleura);
- a 'stove-in' segment of the chest wall.
The fragments of a fractured rib are usually held in place by the muscles between the ribs. After severe injury, a rib fragment may be driven inwards, causing a tear in the covering of the lung with consequent leaking of blood or air into the chest cavity. The lung on that side will then collapse and/or be compressed, resulting in difficulty in breathing. There may be a blue/grey tinge to the skin of the face and lips, and the casualty may cough up frothy blood-stained sputum.
Treatment
Get RADIO MEDICAL ADVICE and get the casualty to expert treatment, or expert treatment to the casualty, as soon as possible.
- place in the half-sitting-up position leaning towards the injured side (Figure 1.62). If both sides are injured, keep in the upright half-sitting up position (Figure 1.63);
- keep the air passage clear. Remove dentures, if worn, and encourage him to spit out any blood, vomit or secretions;
- deal with any sucking wound.
- transport to ship's hospital, or cabin, as soon as possible, but keeping him in the sitting position advised above;
- when in bed, in the correct position, relieve pain but DO NOT GIVE MORPHINE;
- watch for signs of internal bleeding and obstructed breathing.
Unconscious casualty
Transport and later nurse in bed in the unconscious position, lying on the injured side (not the uninjured side) and with a head-down tilt.
Stove-in chest injury
In a very severe injury, multiple fractures of the ribs may lead to a portion of the chest wall being 'stove-in'. That portion contains adjacent ribs which have been fractured at both ends, thus allowing the portion to have free movement independent from and in the opposite direction to the movement of the rest of the rib cage. This is called paradoxical movement and it is an important sign in diagnosis.
Treatment
- give treatment as for multiple fractures of ribs;
- using the flat hand, either the casualty or the attendant should maintain firm pressure over the stove-in portion of the chest wall;
- a pad of folded cloth should be placed over the damaged area and bandaged firmly in place, using wide crepe bandages to encircle the chest. If breathing movements are hindered by the chest bandage, strips of elastic adhesive bandage, which do not encircle the chest, may be used. NOTE: Infections of the lung may appear as a serious complication of any severe chest injury.
Whenever a casualty has to be kept on board, always start a course of antibiotic treatment.
Blast injuries
Explosions cause a sudden and violent disturbance of the air; fires can be started and toxic gases produced.
- men may be thrown down and so injured. Further injury may occur from falling wreckage;
- the blast of air itself may strike the body with such violence as to cause severe or fatal internal injuries;
- cases of burns or asphyxia may occur.
Apart from fractures, wounds, severe bleeding, burns and asphyxia, any combination of the following injuries may be found.
Head
The effect of blast injury to the head is rather like concussion. In some cases there may be paralysis due to spinal cord damage. The patient may be unconscious or he may be extremely dazed. Dazed casualties can be found sitting about, incapable of moving and not caring what is going on. Although apparently to outward appearances uninjured, they do not have the energy, or indeed the will, to move. They will appear confused and disorientated.
- if unconscious, put in the unconscious position immediately. Check for breathing, heart stopped and bleeding;
- if dazed, take them by the hand and lead them to safety. Tell them firmly what they must do. Detail someone to look after them.
Lungs
The blast of air may damage the air sacs and the small blood vessels of the lungs.
- bleeding may take place inside the lungs;
- the patient may be shocked;
- he may have difficulty in breathing. There may be a feeling of tightness in the chest and there may be pain;
- lips, ears and the skin of the face may be blue;
- he may cough up a blood-stained froth;
- take the patient into the fresh air if possible;
- support him in the half-sitting-up position
- loosen tight clothing to allow him to breathe more easily;
- keep him warm and treat for shock;
- encourage him to cough and spit out any secretions produced;
- artificial respiration or assisted respiration may be required if breathing fails or becomes difficult.
PATIENTS WITH CHEST INJURIES MUST NEVER BE GIVEN MORPHINE
Abdomen
Abdominal injury to casualties in the sea can happen as a result of underwater explosions but similar injury can be due to explosions on board ship. The force of the explosion damages the internal organs and causes internal bleeding.
The main features of this type of injury are:
- shock;
- abdominal pain;
both of which may become evident some time after the explosion. If these conditions are found, start a pulse chart. Treatment is that for shock and for internal bleeding.
Transportation
Unless there is danger from fire, explosion or toxic substances, do not move a casualty until suspected fractures have been immobilised and bad bleeding has been stopped. Then check out the best route for transport and lift the casualty gently and carry him smoothly. Every jolt means unnecessary pain.
The method of transport will depend on the situation of the casualty and the nature of the injury. Whatever method is used, try to gain the confidence of the person you are carrying by explaining what you are about to do and then carrying out the manoeuvre in an efficient manner.
Ordinary man-handling may be possible, in which case two helpers carry a casualty without forming their hands into a seat, by each using an arm to support the casualty's back and shoulders and each using his spare hand to support the casualty under his thighs.
If conscious, the casualty may help to support himself with his hands on the shoulders of the helpers (Figure 1.65).
 Position taken up
Position taken upwhen man-handled, or
a fourarm seat is being used;
in the former instance
two arms are at the back
of the patient and only
two are under his thighs.Figure 1.65
The four-handed seat can be used when a heavy person has to be carried. The disadvantage of this type of seat is that the casualty must be able to co-operate and to hold on with both arms around the shoulders of the two men carrying him. It cannot be safely used to negotiate ladders (Figure 1.65).
The hands should be placed as in Figure 1.66.
One advantage of the three-handed seat (Figure 1.67) is that one arm and hand of a helper is left free and can be used

Figure 1.66

Figure 1.67
either to support an injured limb or as a backsupport for the casualty. According to the nature of the injury, it is decided which of the two helpers has the free arm (Figures 1.68 and 1.69).
The fireman's lift which should not be used unless the helper is as well built as the casualty is especially useful when you have to move a man by yourself and need the use of your right hand for holding on to a ladder. Roll the patient so that he is lying face downwards, lift him up so that, when you stoop down, you can put your head under his left arm (Figure 1.70).

Figures 1.68

Figures 1.69

Figures 1.70
Steady yourself and then stand upright, at the same time shifting his weight so that he lies well balanced across the back of your shoulders (Figure 1.72). Hold the casualty's arm above the wrist. In this position it is easy to carry the patient up a ladder as one hand is free to grasp the rail (Figure 1.73).

Figure 1.71

Figure 1.72

Figure 1.73

Figure 1.74

Figure 1.75
As a last resort, the drag-carry method may have to be used in narrow spaces, particularly where there is wreckage following an explosion and where it may be possible for only one man to reach a trapped casualty and to rescue him. After initial rescue, two men may be able to undertake further movement through a narrow space. The method is demonstrated in Figures 1.74 and 1.75. Ensure that the casualty's wrists, which are tied together, do not interfere with any breathing apparatus the rescuer may be wearing, and safeguard the casualty's head with a bump hat if possible.
Neil Robertson stretcher
This particular type of stretcher is shown in Figure 1.76. It is a simple device for moving a casualty safely from a difficult place where the ordinary stretcher with stiff poles would be useless. Other patterns of rescue stretcher are available but all aim to achieve the same purpose. The casualty is enveloped in a protecting but somewhat flexible case, so that he takes up as little room as possible. The stretcher can be bent slightly in turning sharp corners in narrow passages, as when being hoisted up the ladder ways from engine-rooms, or through the hatches of cargo tanks.
The stretcher is made of stout canvas, stiffened by wooden slats (Figure 1.76). The portion 'A' takes the head and neck, which are steadied by a canvas strap passing over the forehead. Thus, the head of an unconscious patient can be steadied.
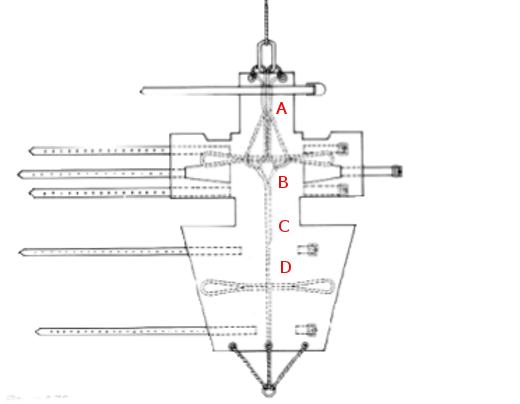
Figure 1.76
The portion 'B' is wrapped round the chest, notches being cut on which the armpits rest. This part has three canvas straps which are used for fastening the stretcher round the chest. The portion 'D' folds round the hips and legs down to the ankles. It is secured by two canvas straps.
A central backbone of stout rope passes along the under surface. This has two beckets passing out from it on either side which can be used as handles, for carrying the patient or for securing tackles when he is slung horizontally.
At the head end, the rope ends in a grommet which takes extra purchase from two brass eyelets let into the canvas. At the foot end of the rope is a galvanised iron ring which is secured to the stretcher by a span going to brass eyelets in the canvas. When more rigidity in the stretcher is required, as in moving those with injuries to the back, a couple of broom handles, slipped through the ropes underneath, will fulfil this purpose admirably.
Some stretchers have a rope about 9 ft long fixed to the galvanised ring at the foot end. This is a steadying rope for use in craft below, or on quay, when the patient is lowered over the side of the ship. When the patient is carried about the ship, this rope can be passed under the various straps to keep it from trailing on the deck or otherwise getting in the way.
The patient should be lifted on to and secured in the stretcher as shown in Figures 1.77 to 1.80.
Cases of fracture of the spine or other back and pelvic injuries should be transferred to the stretcher as directed under spinal injury.
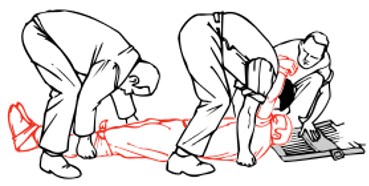 Getting ready to lift the casualty
Getting ready to lift the casualtysufficiently for the Neil Robertson
stretcher to be slid under him.
With only three attendants, the wrists
of an unconscious patient have to be
tied together - but not tightly.Figure 1.77

Lower the patient slowly - if he is unconscious, support his head.
Figure 1.78
 Ensure patient's armpits are
Ensure patient's armpits arein the correct place before
you finish lowering him.
Figure 1.79

Strapped up - the arms can be strapped inside or outside
the chest section of the stretcher, depending upon the injuries.
Figure 1.80

but keep the head section level
with the chest section
if the neck may be hurt.
Figure 1.81
The patient should be carried by four men, if possible (Figure 1.81). At difficult corners, the stretcher should be lowered at the foot end, and the casualty passed by two of the men to the others. The carry can then be resumed by the four bearers.

Hoisting a casualty through a hatch
(see also Figure 1.83).
Figures 1.82
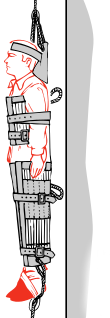 Moving a casualty vertically.
Moving a casualty vertically.Note:
to steady the stretcher, a rope
goes from the foot of the
stretcher to a seafarer below.
Figures 1.83
When passing the casualty through a narrow hatch, or lifting him up over a height, or lowering him to a boat alongside, put the lifting hook or a rope through the grommet at the head end and a further steadying rope through the galvanised ring at the foot end (Figures 1.82 and 1.83).
Moving an unconscious casualty
If possible, carry an unconscious casualty in the unconscious position and always with a head-down tilt. The tilt is also necessary when carrying a casualty suffering from shock or loss of blood.
Further information
Contact MCA's health and safety branch
Telephone: 0203 8172504 or 0203 8185138Medical Administration Team
Maritime and Coastguard Agency
Spring Place
105 Commercial Road
Southampton
Hants
SO15 1EG
UsA DataErol.
 Where Captains meet Dock Owners
Where Captains meet Dock Owners